Get more done with less stress and pay only $12/hour.
A virtual medical assistant can help!
Get more done with less stress and pay only $12/hour. A virtual medical assistant can help!
Businesses thrive with solutions that drive success and transformation. Clients achieve their goals, streamline operations, and see real results. Join them and experience the difference today!
Join the countless satisfied physicians who trust our proven solutions, backed by an extensive arsenal of happy clients enhancing their practices.











We were overwhelmed with calls while our staff focused on in-clinic patients. Portiva came highly recommended, and since bringing on Jennifer as our Virtual Front Desk Receptionist, things have run much more smoothly.
I am currently employing and managing 3 virtual medical assistants in various roles including billing, population health and back office. These exemplary individuals are smart, self-starters who can be trained to perform new tasks.
Prior to Portiva, I used another virtual staffing agency and I was not happy with the candidates or the service. Portiva does an excellent job pre-screening qualified candidates that meet the requirements of the job.
It has been a pleasure working with Portiva and their VMAs. Before working with them, we faced challenges managing the increasing workload that came with our growth, especially with limited on-site space.
Discover how our dedicated clients have achieved their goals and transformed their businesses with our expert solutions. Join the ranks of satisfied customers and experience the difference for yourself.
Healthcare providers today face increasing challenges with complex insurance rules, evolving coding standards, and frequent claim denials. With Portiva’s professional medical billing services, practices can streamline their revenue cycle, minimize unpaid claims, and dedicate more time to delivering quality patient care.
Maximize your practice’s financial performance with Portiva’s end-to-end billing solutions. Backed by years of healthcare expertise, our expert billing teams help reduce revenue leakage, lower administrative costs, ensure compliance, and provide patients with a seamless billing experience.


At Portiva, we provide comprehensive medical billing services tailored to optimize your entire revenue cycle. From solo practices to large healthcare networks, our deep expertise in billing and revenue cycle management delivers accuracy, compliance, and maximum reimbursement.
Our experienced billing team streamlines complex processes so you can concentrate on exceptional patient care. With advanced billing technology, knowledgeable account managers, and proven best practices, we manage everything from claim submission and payment posting to denial follow-ups. Partnering with Portiva gives you a scalable, cost-efficient solution that lowers administrative workload, reduces claim denials, and drives consistent revenue growth.
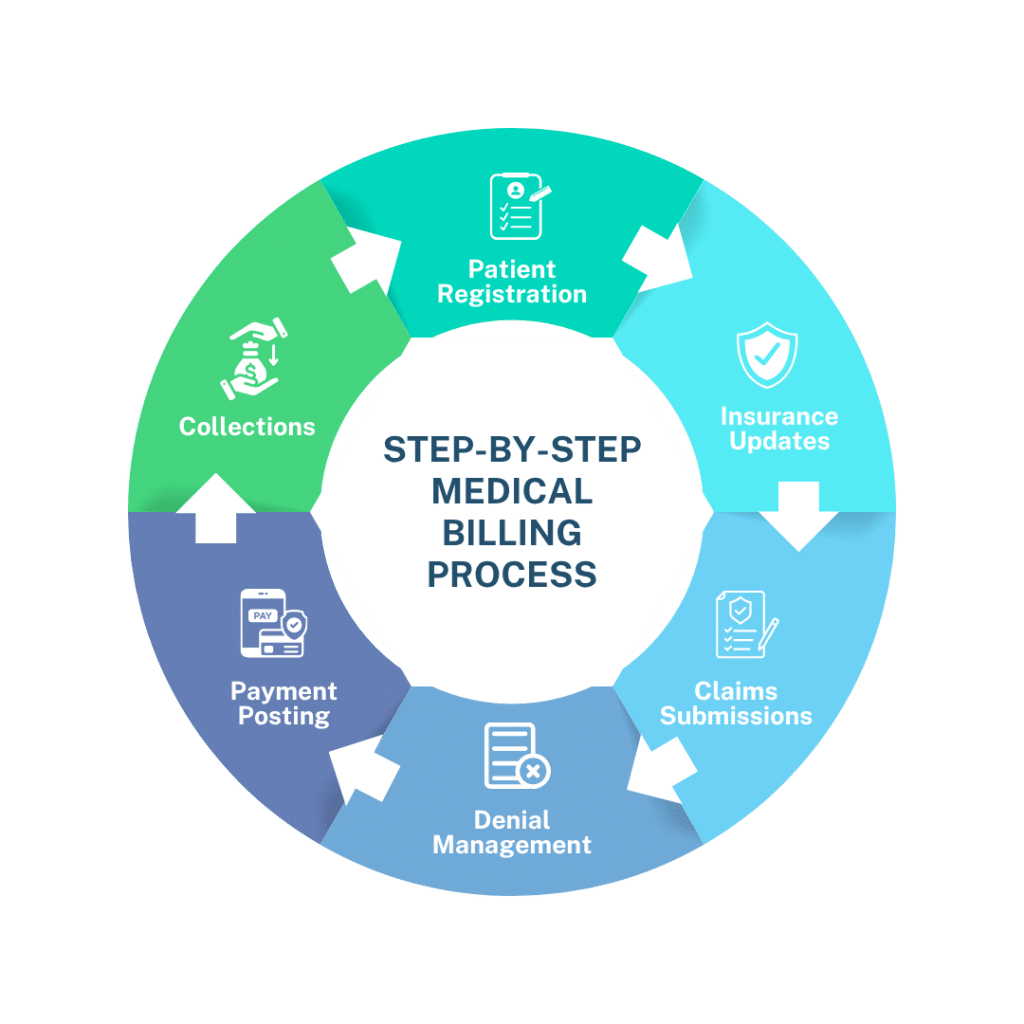
Portiva medical billing services encompass the entire process of submitting, following up, and collecting payments from insurance companies and patients. This includes coding, insurance verification, claim submission, denial management, payment posting, patient invoicing, and reporting.
At Portiva, medical billing is part of the broader RCM workflow from patient registration through final collection. Strong RCM ensures fewer claim denials, faster payments, and improved cash flow.
Our Medical Billing Services Include:
Streamline tasks, cut costs, and focus more on your patients.
Outsourcing billing lets you free staff from complex tasks, reducing overhead and administrative errors.
| Component | What your medical billing service should offer |
|---|---|
| Coding & Documentation | Certified coders who work with ICD-10, CPT & HCPCS, ensure accurate documentation |
| Claim Submission & Tracking | Electronic claims, submission to proper payers, tracking, and follow-up on delays |
| Denial Management & Appeals | Identification of denials, root cause analysis, resubmissions, and appeals |
| Insurance Verification & Auths | Confirm patient eligibility and obtain prior authorizations to avoid denials | Payment Posting | Post payments, reconcile with patient accounts, identify underpayments | Patient Billing & Support | Bill patients, manage statements, answer questions, offer payment plans if needed | Analytics & Reporting | Regular financial reports, KPIs, insight into denials, aging reports, and cash flow projections | Security & Compliance | HIPAA compliance, data security, audit controls, privacy protection |
Understand your billing processes, software (EMR/EHR), specialties, and pain points.
Connect with your EMR / practice management system, set up secure data exchange.
HIPAA-compliant dental admins protect patient data and deliver trusted support.
Proactively prevent denials by verifying insurance, reviewing documentation; handle appeals.
Monthly/weekly reports; analytics track metrics like days in AR, denial rate, clean claim rate.
We provide dedicated support for all medical specialties, ensuring comprehensive and tailored solutions.
The medical billing industry is constantly evolving, with new payer rules, compliance standards, and coding updates creating challenges for providers. Practices that try to manage billing in-house often face high denial rates, delayed payments, and administrative burdens. Partnering with professional billing experts helps reduce these risks and ensures smoother revenue cycle management.

Medical billing covers the full financial workflow—submission of claims, insurance follow-ups, patient billing, payments. Medical coding is the process of translating diagnoses, procedures, and services into standardized codes (ICD-10, CPT/HCPCS) which are then used in billing.
Medical billing has become increasingly complex, and healthcare providers face several pressing challenges.
One of the biggest hurdles is building a reliable team of expert billers and coders. With the ongoing labor shortage in the U.S., finding, training, and retaining qualified staff is both time-consuming and costly.
This staffing gap leads to inefficient onboarding processes and higher administrative costs. Without an experienced and cohesive team in place, billing operations are prone to errors and delays, making the entire revenue cycle less secure. The result? Providers lose valuable income that should have been collected.
In addition, poor coding practices remain a significant issue. Inaccurate or inconsistent coding often results in claim denials, delayed reimbursements, and lost revenue. Over time, these small mistakes compound, putting unnecessary financial strain on practices and healthcare organizations.
Accurate coding is crucial for clean claims, with over 50% of denials linked to coding errors. Improper coding directly causes lost revenue, and constant code changes make it hard for busy staff to keep up.
Physicians facing EHR challenges may also miss codes or documentation, increasing denial risks. That’s why expert coders and billers are essential for boosting revenue.
With these challenges, the outsourced medical billing industry continues to grow by 12% annually, helping providers reduce errors and secure payments faster.
Yes. We integrate with major EMR / PMS systems. We can also handle claims submission via clearinghouses or directly to payers as required.
Costs depend on volume, specialty, payer mix, and complexity. Typical models include percentage of collections, per claim, or hybrid. We’ll provide a transparent quote after reviewing your practice’s specifics.