Prior Authorization Prescription: What Patients and Providers Must Know
Unlock Precision: Your Doctor’s Companion for Prior Authorization Prescriptions. Lock in Your Appointment Today!
How Can A Virtual Medical Assistant Help Your Practice?
See how Portiva is making a real difference in medical practices through our clients’ experiences. Watch this short video to see the impact for yourself, and let’s talk about how we can help streamline your operations and improve patient care today!
Table of Contents
Prior Authorization Basics
Prior authorization is a technique employed by health plans and insurance companies to evaluate whether a prescribed drug or a medical service will be paid. This restriction is expected in some sense because level of control is being exerted in what is perceived to be for the greater good. It is designed to encourage patient safety, cost effective therapy, and prevent misuse of medication or abused drugs.
But prior authorizations, if not done well, have the potential to create substantial burdens for both providers and patients, both in streamlining workflows and in reducing the delays to care – enhancing the level of frustration in the healthcare system.

What Is A Prior Authorization Prescription?
A prior authorization prescription is one where it is needed special consent from a health plan or insurance plan before it can be given out or paid back. The prescription medication is subject to an authorization decision by the insurance company in advance which determines eligibility. This prerequisite is typically placed on branded pharmaceuticals, costly treatments, medications prescribed off-label, or drugs that are over-used or over-exploited.
In some instances, prior approval may be required owing to particular patient medical conditions or if the medication fulfills cosmetic rather than therapeutic purposes.
What Is The Reason For Health Plans Require Prior Authorization?
There are multiple reasons why health plans utilize prior authorization programs:
- Patient protection: To make sure that the patient will not be harmed be the medication ordered.
- Economic control: To incentivize the use of alternative medications that are less costly and still effective.
- Misuse prevention: Particularly for drubs that are prone to abuse or are very addictive.
- Age restrictions: Some medications need to be restricted by certain age groups due to safety issues.
- Specialty drug oversight: Many specialty or biologic medications need a lot of supervision.
Prior authorization requires a detailed letter of reason and appropriate documentation from the doctor that makes the proposal. This enables the insurance company to review whether the drug recommended by the prescribing physician is indeed needed. Healing procedure with prior authorization.
How the Prior Authorization Process Works
It begins when a healthcare provider submits a prior authorization request to the insurance company.
This request often consists of:
- Medical History Documents
- Clinical justifications for the medication
- Details derived from the patient’s eHealth record.
After the documents are sent, the insurance company analyzes the request using its own business rules, coverage policies, and the documentation associated with the patient’s health plan. This process ultimately leads to a coverage determination, where the insurer decides whether the requested medication or service is covered under the patient’s health plan. The prior authorization decision is made based on these factors, and the work cycle or the length of time it takes to process prior authorizations can range from several hours to a few business days.
In cases where the request has been granted, the pharmacy is able to supply the requisite medicine. It is also possible that an appeal claim may be filed by the patient or the healthcare provider if the request was denied.
Common Reasons Medications Require Prior Authorization
Some medications are more likely to require prior authorization including:
- Excessive expense: Biologics or medications that have just recently been released are examples of this.
- Availability of generics: More affordable and effective alternatives exist.
- Limited medical necessity: Medications prescribed for cosmetic reasons.
- Restricted use cases: Drugs approved only for specific medical conditions or age ranges.
- Concerns about dosage: Medications commanding higher than average guidelines for dosage prescriptions.
Health plans formulate their formularies through formulary as an example of clinical evidence, FDA approval, and cost-effective treatment planning. When a prescribed medication falls outside these guidelines, a prior authorization requirement is triggered to ensure that the drug meets the necessary standards for approval.
See What Our Clients Have to Say!
Learn how our expert solutions have helped businesses achieve their goals and drive success. Join our satisfied customers and experience the difference today!
Boost your Efficiency with
Portiva's Virtual Medical Assistant Services
Portiva’s Virtual Medical Assistant Services help healthcare providers streamline administrative tasks, improve efficiency, and enhance patient care all while reducing workload and costs.
Medical Assistant
Insurance Verification
Medical Receptionist
Prior Authorization
Medical Scribe
Dental Assistant
Medical Transcription
Executive Assistant
Medical Billing
Medical Billing
The Workload That Comes With Prior Authorizations For Providers
Healthcare providers usually believe that the administrative burden related to prior authorization is especially high. For example, the American Medical Association states that physicians and their office staff spend a significant amount of time each week dealing with prior authorization requests, which frequently include phone calls/ faxes and other forms of documentation.

As a result, this time consuming process may:
- Stagnate the patient’s care
- Overload small practices
- Oftentimes place a mentally exhausted provider into a situation that leads to burnt out.
- Develop false rejections
- Result in provider burnout
With the use of digital health records systems, it is possible to add some automated prior approval processes, and authorization review systems can still be quite cumbersome. The building of unique standards from the various insurance companies does create a problem for providers in regards to meeting the ever-changing needs setting the requirements.
Impact on Patients: Delays and Denials
For patients, having to jump through hoops like prior authorizations really feels like more than an annoyance it feels like an extra barrier to getting the care they need. A survey by the AMA found that a truly huge number of physicians close to 94% are reporting delays in getting care because of formularies that ask for authorizations first.
Here’s how patients are affected:
- Treatment delays: Especially in cases involving urgent medication needs where an urgent request for prior authorization is necessary to avoid interruptions in care.
- Out-of-pocket costs: If the drug is denied and no substitute medication is approved.
- Appeal process stress: Navigating process of getting decisions overturned can be really stressful and grueling without help.
- Missed doses: Gaps in treatment can worsen health issues.
People enrolled in Medicare Advantage plans or those using medicare’s prescription drug coverage may face even stricter requirements for prior authorizations. This usually kicks in for specialty drugs or treatments that carry higher coverage levels and cost a bit more.
Which Prescription Drugs Are Most Affected?
Some of the most prevalent examples of drugs require prior authorization include:
- Widely used under non-approved indication and off-label uses
- Costly injectables and biologics
- Pain medications with heavy abuse potential
- Cosmetic weight loss, hair growth, and acne medications
Prescription drugs included on a health plan’s formulary are listed in order of tiers. Higher-tier drugs are more likely to be specialized in and cost expensive, thus demanding prior authorization.
The Involvement of Electronic Health Records Systems In the Workflow
The activation of EHR has resulted in the automation of certain sections within the prior authorization workflow. EHR systems can keep specific details pertaining to plans, warn providers about authorizations, and even obtain prior authorization requests electronically from the providers’ offices to the insurance company.
The advantages are as follows:
- Improved documentation
- Reduced claim denials
- Quicker approval times
- Better tracking of prioritized requests
Some insurance providers and EHR systems do not fully integrate together. Due to some prior authorization applications still require paper documents to be submitted, additional work is created.
Prior Authorization and Medicare Part D
Medications that are included in the Medicare Part D plans come with harsh prior authorization clauses. There are individualized rules to each health insurance plan especially with regard to the formulary, meaning the specific documents associated with the health plan need to be verified by the patients in detail.
The salient issues include:
- Determining coverage before some medications are dispensed is essential.
- Certain elderly patients may face restrictions.
- There are timelines for appeals that need to be respected so that preemptive action can be taken without hassles.
- An urgent review process can be requested under medical justification.
Patient can coordinate with doctors to avoid any delay resulting from lack of complete documentation that is necessary.
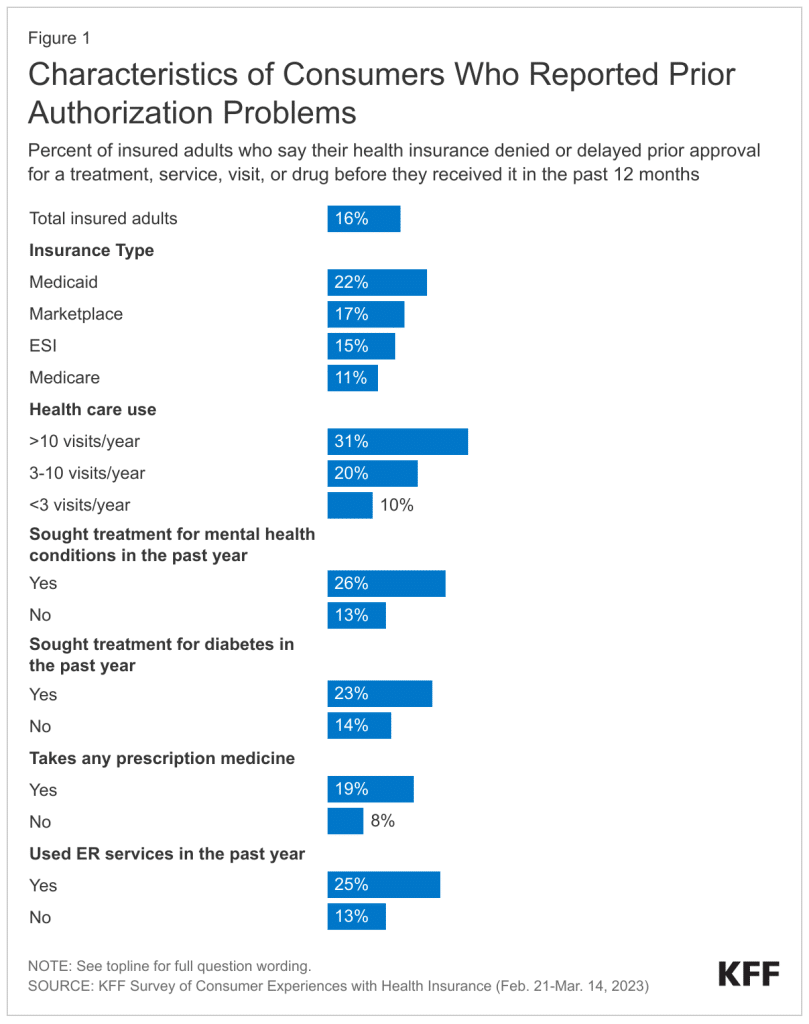
Characteristics of Consumers who Experience Prior Authorization Problems
Key Insights:
- Medicaid enrollees and high healthcare users face the highest rates of prior authorization issues.
- Mental health and emergency care are associated with significantly more delays/denials.
- Federal law prohibits prior authorization for emergency services, yet 25% of ER patients still report problems.
Procedure for Appeal Following a Denial of Prior Authorization
A denial of prior authorization request, requires the decision to be challenged through an appeal process and there is a way out.
- Go through the denial notice for specific reasons.
- Gather additional evidence such as EHR notes and justification for medical necessity.
- Request a determination of coverage or formally appeal within the time limit.
- If the appeal gets denied, access an external review by the health insurance or the relevant state agency.
It is important for patients to retain every piece of correspondence and work alongside the physician’s office in defending the appeal.

The Need for Reform in Prior Authorization Systems
People who do doctors’ visits and folks who use medical care both think the current system of reviewing requests ahead of insurance paying is confusing and hard. Originally meant to make patients safer and control healthcare spending, in practice these efforts usually end up just the opposite.
Key reform ideas include:
- Standardization: Uniform forms and procedures across insurance companies.
- Transparency: Clear criteria published in plan documents.
- Automation: Expanded use of digital health record integrations.
- Accountability: Monitoring for incorrectly denied cases.
- Exemptions: Fast-track options for trusted providers with a history of compliant prescribing.
Nonprofits like the good folks at the American Medical Association are working on making health plan rules for treatment less tiresome for health providers. These folks are really trying to pump up how fast care gets, so patients get quick access to what they need.
Best Practices for Reducing Lags in the Prior Authorization Procedure
Here are some best practices healthcare providers and patients can follow to reduce delays in the prior authorization process:
- Timely submissions: Submit the prior authorization request immediately after the prescription drug is written.
- EHRs: How far along can submission automation be done through the provider’s EHR system?
- Confirm documentation correctness: All relevant information concerning health issues and the treatment approach should be included.
- Understand what is on offer: Be familiar with the health insurance’s formulary of the list of medications requiring prior authorization.
- Look into other options: Inquire whether there is another drug that does not require any authorization.
Conclusion: Streamlining the Prior Authorization Process in Healthcare
The prior authorization process in healthcare is both complex and often inefficient. Its intent is to contain costs, prevent misuse of medication, enhance safety, and ensure the wellbeing of patients. On the other hand, excessive administrative work, variability in decision-making, and slow response times quickly complicate service delivery.
Reforms geared towards improving efficiency need to be prioritized. Utilizing modern solutions, advocating for procedural standardization, and calling for transparency can assist in the swift access to medication for patients.
If you are facing a prior authorization hurdle, you and your loved ones need to remain vigilant and collaborate with the healthcare team to mitigate the delays that come from bureaucracy.
- How is the concept of prior authorization interpreted in pharmacy?
- What is involved in appealing a decision on a denied prior authorization?
- How is the concept of prior authorization interpreted in insurance?
- How is the concept of prior authorization interpreted when it comes to prescriptions?
- Is it a common practice to seek prior authorization from Medicare for surgery?
- How is the concept of prior authorization interpreted in Medicaid?
- How can collaboration between healthcare providers speed up prior authorization for medication?
- How do Medicare guidelines address prior authorization for healthcare services?
- What advice do experts give to manage expectations regarding prior authorization timing for medication?
- What specific medical information is crucial for the Prime Therapeutics prior authorization form?
- How does the complexity of a patient’s condition affect the medication prior authorization process?
- What is involved in appealing a decision on a denied prior authorization?
- What strategies can healthcare professionals use to manage Medicare prior authorization for multiple patients?
- How can healthcare advocacy groups influence reforms in the medical prior authorization process?
- What strategies can be used to manage multiple prior authorizations with Express Scripts?
- How do denials of preauthorization or precertification reflect on healthcare policy and practice?
- What strategies can healthcare providers use to manage prior authorization requirements effectively?
- Can you explain how the healthcare system’s efficiency is affected by referrals compared to prior authorizations?
- How can healthcare advocacy groups influence reforms in the insurance prior authorization process?
- How does the complexity of a medical case affect the prior authorization process?
- How does the complexity of healthcare services affect the prior authorization requirements?
- What measures are being taken to address delays in the prior authorization process for medications?
- How does the complexity of a patient’s condition affect the prior authorization process?
- What are the professional development opportunities for nurses in the prior authorization field?
- How do prior authorization pharmacists navigate ethical considerations in their work?
- What are the career advancement opportunities for remote prior authorization specialists?
- What career progression opportunities exist for individuals in the prior authorization specialist role?
- How is the concept of prior authorization interpreted in pharmacy?
- How to navigate the appeal process for a denied prior authorization?

