Best Prior Authorization Companies
A Guide for Healthcare Practices
Partner with the best prior authorization companies today to streamline approvals, reduce delays, and give your patients the care they deserve.
How Can Prior Authorization Remote Help Your Practice?
See how Portiva is making a real difference in medical practices through our clients’ experiences. Watch this short video to see the impact for yourself, and let’s talk about how we can help streamline your operations and improve patient care today!
Table of Contents
Navigating the prior authorization process is one of the most persistent administrative challenges in healthcare. Clinics, hospitals, and independent practices spend countless hours managing prior authorization requests, often leading to unnecessary delays in patient care. To overcome these hurdles, many providers now partner with the best prior authorization companies that deliver powerful prior authorization capabilities and seamless integration with existing systems. Choosing the right digital health solutions helps medical practices save time, improve approval rates, and prevent lost revenue.
Why Prior Authorization Matters
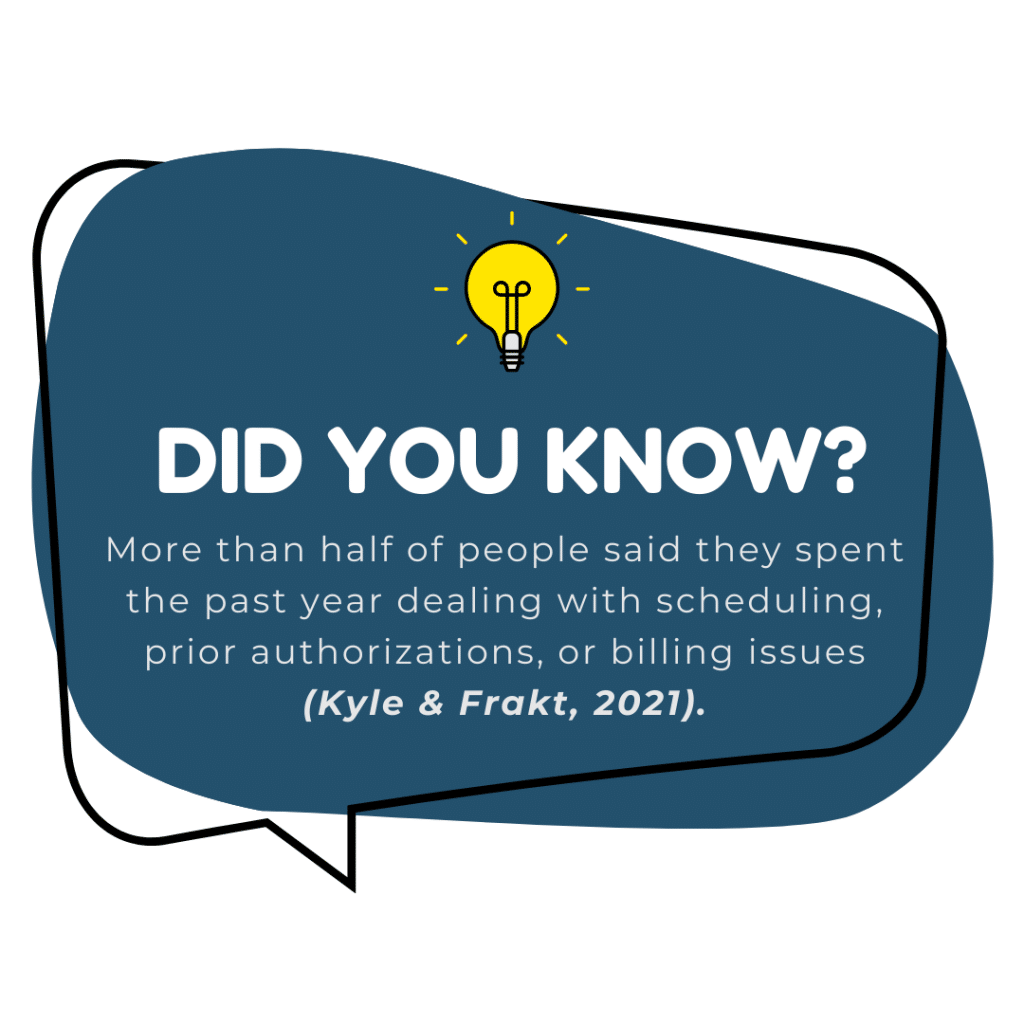
Prior authorization is designed to ensure medical necessity documentation before patients receive certain medical services. While the goal is to maintain quality, the reality is often burdensome. Healthcare providers face back and forth phone calls with insurance providers, payer submissions, and claim denials when prior authorization documentation doesn’t meet payer requirements.
These issues slow down patient access to essential healthcare services. Health systems and multi specialty practices report that manual prior authorization remains time consuming, with authorization process delays impacting patient satisfaction. Efficient solutions are now critical for medical practices and hospital networks aiming to streamline workflows.
The Shift Toward Digital Prior Authorization Solutions
Traditional manual prior authorization required phone calls, faxed forms, and repetitive eligibility checks. This outdated prior authorization method created administrative burden, slowed clinical workflows, and reduced cash flow.
In contrast, electronic prior authorizations supported by integrated delivery networks and digital health solutions bring efficiency. Prior authorization modules integrate seamlessly with payer systems, ensuring providers can obtain approval faster and with fewer errors. With the right tools, practices and health systems can reduce expenses, save time, and increase approval rates.
Key Features of Effective Prior Authorization Services
The top prior authorization companies offer more than basic request handling. They integrate with existing systems to make processes smooth and user-friendly, especially when dealing with high volumes of prior authorization requests. Many prior authorization companies also provide analytics and reporting tools that help providers spot denial trends.
Features often include clinical decision support, automated reporting tools, and peer reviews for complex medical necessity documentation. Many providers now rely on electronic prior authorizations to simplify these steps and reduce prior authorization delays. These services integrate seamlessly with large hospital systems, health systems, and independent practices alike, offering a user friendly interface to manage requests.
Another important feature is the ability to generate market insights. Advanced report generators help health systems make informed decisions and identify patterns in claim denials. By analyzing patient data, providers and health systems can adjust workflows and improve approval rates across specialties, showing the true value of modern prior authorization services.
What Our Clients Say About Us!
Discover how our dedicated clients have achieved their goals and transformed their businesses with our expert solutions. Join the ranks of satisfied customers and experience the difference for yourself.
Boost your Efficiency with
Portiva's Virtual Medical Assistant Services
Portiva’s Virtual Medical Assistant Services help healthcare providers streamline administrative tasks, improve efficiency, and enhance patient care all while reducing workload and costs.
Medical Assistant
Insurance Verification
Medical Receptionist
Prior Authorization
Medical Scribe
Dental Assistant
Medical Transcription
Executive Assistant
Medical Billing
Medical Billing
How Prior Authorization Companies Support Healthcare Providers
Partnering with specialized prior authorization services eases one of the most persistent administrative challenges in modern healthcare. These prior authorization services allow providers to reallocate staff hours from admin tasks to patient care.
By outsourcing, medical practices avoid the back and forth of payer rules and payer submissions. These services simplify the prior authorization process, reduce administrative strain, and make it easier for providers to manage prior authorization efficiently while preventing lost revenue and ensuring compliance with payer systems.

Comparing Top Prior Authorization Companies
Choosing the right partner requires more than looking at cost. Healthcare providers must efficiently search vendors, compare solutions, and find services that integrate seamlessly into their clinical workflows.
Top prior authorization companies offer scalable solutions for large hospital systems, multi specialty practices, and independent clinics. They use digital health solutions to reduce time consuming manual steps, while providing clinical decision support and reporting tools that help health systems make workflows more efficient.
Two reliable resources to explore industry performance are:
American Medical Association (AMA) – Their research highlights how prior authorization impacts patient care and provider efficiency (AMA Resource).
Centers for Medicare & Medicaid Services (CMS) – CMS studies provide insights into electronic prior authorizations and how digital solutions improve approval processes (CMS Resource).
Benefits for Different Types of Practices
Hospital networks deal with high volumes of prior auth requests daily. Without efficient prior authorization systems, approval delays can lead to lost revenue, reduced patient access, and significant administrative burden. Integrated prior authorization services not only streamline workflows but also demonstrate how scalable prior authorization services enhance overall financial performance.
For smaller practices, prior authorization can consume disproportionate time. With limited staff, paper-based prior authorization can easily become overwhelming. Outsourcing to prior authorization companies allows providers to focus on patient care while still working efficiently to obtain approval from payers.
Managing requests across multiple specialties adds complexity. Prior authorization solutions with robust reporting tools help multi specialty practices streamline requests, reduce errors, and avoid claim denials. These prior authorization solutions also ensure consistency across departments, saving time and maintaining smooth cash flow.
Conclusion: Transforming Patient Care with the Best Solutions
Prior authorization remains one of the most enduring administrative challenges in healthcare. But with the right digital health solutions, providers can reduce expenses, improve approval rates, and focus on patient care. By partnering with the best prior authorization companies, practices gain powerful prior authorization capabilities, seamless integration with current systems, and relief from the time consuming approval process. Now is the time to choose smarter solutions that transform healthcare delivery and enhance patient access.
Ready to streamline your prior authorization process? Explore powerful prior authorization solutions at portiva.com today and take control of patient care efficiency.